We Need to Talk About Menopause …

Menopause is complex and individual — it involves a wide range of physical and emotional changes, not just hot flushes.
Queer and gender-diverse people experience menopause too — their experiences are valid but often overlooked in mainstream health advice.
Inclusive, affirming care matters — everyone deserves informed, respectful, and LGBTIQ+friendly support during menopause.
For some LGBTIQ+ people, menopause can be a time of reflection and relief. For others, it can be a rollercoaster of challenging symptoms and confusion.
Whether you’re already deep in hot flush territory or just starting to notice changes in your cycle, here’s what’s going on in your body, what to expect, and what you can do about it.
What is menopause, anyway?
Here’s the deal: menopause isn’t just a series of hot flushes and mood swings before life goes back to normal. It’s officially defined as 12 months in a row without a period. But the messy, confusing, often chaotic bit leading up to it is called perimenopause.
For most women and people assigned female at birth (depending on whether you’re taking gender-affirming hormone therapy), menopause usually kicks in between 45 and 55. The average? Around 51 or 52. But it can hit earlier if you’ve had your ovaries removed — which, spoiler alert, doesn’t mean your body is going to politely skip the symptoms.
What’s causing it?
It all comes down to hormones. Menopause is driven by a natural fall in hormones (e.g. oestrogen and progesterone). As these hormones levels change, your body reacts in all sorts of ways.
While trans women do not go through menopause, if they are taking gender-affirming hormone therapy, they might experience symptoms which are like menopause such as mood changes or night sweats. These might happen if hormone therapy is reduced or stopped.
I’ve heard about hot flushes, but what are the other symptoms?
While the infamous hot flushes and night sweats have long been associated with menopause, there are dozens of symptoms you can experience, which include both physical and mental and emotional symptoms:
Physical symptoms may include:
- irregular periods
- hot flushes
- night sweats
- joint aches and pains
- sore breasts
- itchy, crawly or dry skin
- exhaustion and fatigue
- dry vagina
- headache or migraine
- sleep problems
- bloating
- urinary problems
- weight gain.
Mental and emotional symptoms may include:
- feeling irritable or frustrated
- feeling anxious
- difficulty concentrating
- brain fog
- forgetfulness
- mood changes including lower mood
- low libido or interest in sex
- feeling you can’t cope as well as you used to.
About 15% of people going through menopause do not experience any of the common symptoms. For others, it can be years of managing symptoms that disrupt work, sleep, sex and daily life.
Sounds daunting, how can I manage it?
Fortunately, there is help! For many, Menopausal Hormone Therapy (MHT) is a safe and reliable way to ease common menopause symptoms. It is low risk when started between the ages of 50 and 60, or within 10 years of your final period. Additionally, non-hormonal therapies can also ease symptoms. It’s about finding what fits our body, our needs, and our comfort zone.
Sex, intimacy and changing bodies …
Menopause doesn’t mean the end of sex — but it might mean a different relationship to pleasure, sensation, and desire.
You might notice vaginal dryness, changes in libido, or discomfort with certain types of touch. For some people, this is frustrating. For others, it’s a chance to explore new kinds of intimacy, or reconnect with their body on different terms.
There are options like vaginal lubricants and moisturisers, pelvic physio, or low-dose vaginal oestrogen creams and pessaries (if it’s right for you) — but what matters most is tuning in to what you want, not what you think you should want. You deserve pleasure that works for you.
And what about testosterone therapy?
Yep, it’s a thing. Testosterone therapy can be a helpful option during menopause, especially for dealing with low libido. In Australia, there is a prescribable testosterone cream specifically for low sexual desire following menopause.
Lately there has been a lot of attention around the supposed benefits of testosterone. While some of the information sounds promising, not all of it is backed by solid science. It’s important to talk with a healthcare provider about your symptoms so they can help make sure you get the right care that’s informed, inclusive and focussed on your needs.
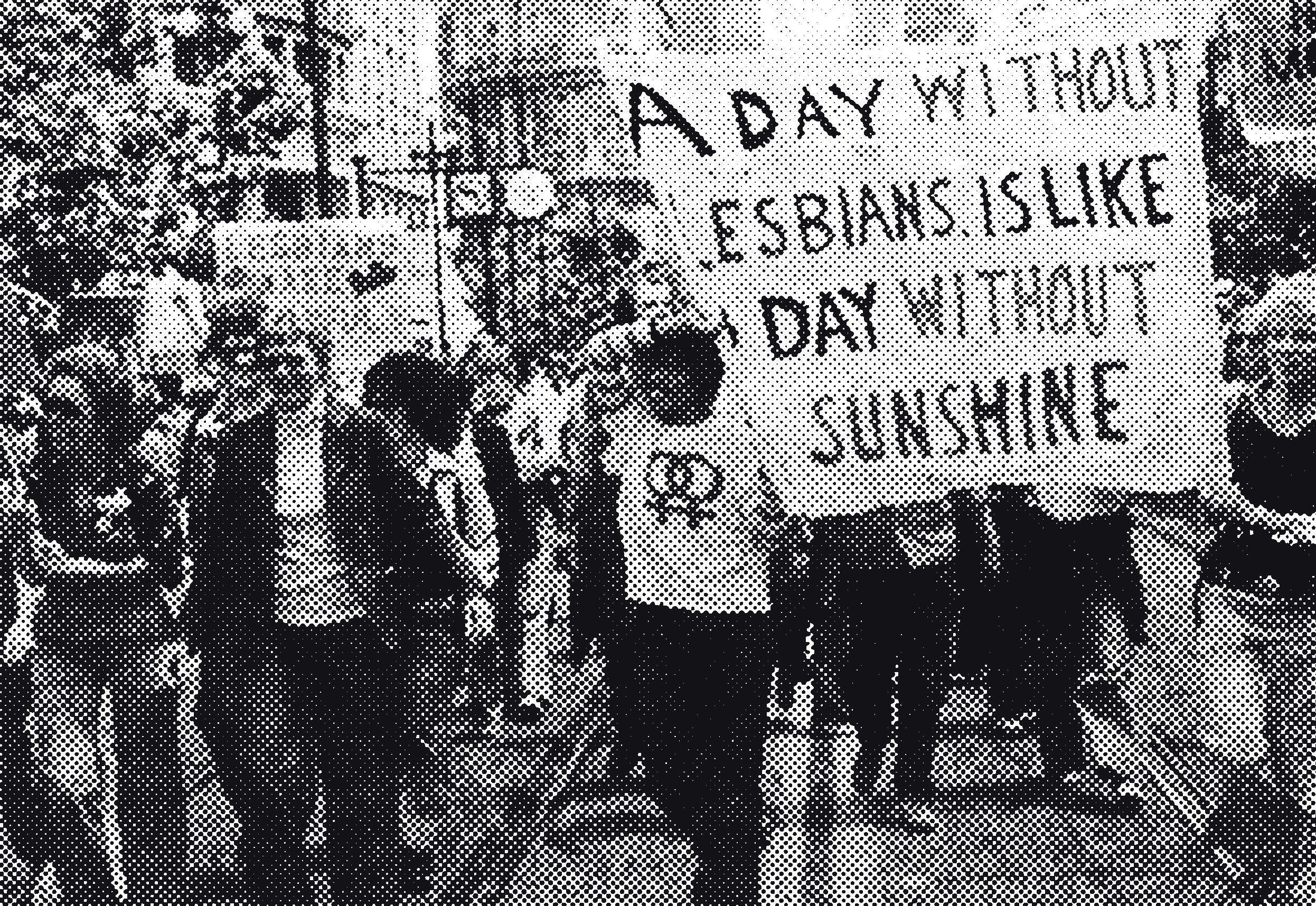
Queer and menopausal? You’re not alone.
Mainstream menopause advice often comes from a heteronormative place, which centres around cisgender identities and traditional family structures. But queer women, non-binary folks and trans people also go through menopause – and we bring our own experiences, challenges and resilience to the table.
For example:
- You might feel invisible in medical settings — or worse, dismissed altogether.
- You may have had a complicated relationship with your reproductive health, especially if you’ve avoided or delayed gynaecological care due to trauma or discrimination.
- You might have a chosen family rather than a traditional partner-and-kids setup — and that matters when it comes to support.
- Menopause might trigger dysphoria, for some trans masc and non-binary people,
- Your partner may also be going through menopause which can come with its own set of challenges
The point is: there’s no one-size-fits-all menopause, and your queer experience is completely valid.
Finding queer-affirming care
If you feel dismissed, misgendered, or talked over – that’s not okay. You deserve care that sees you.
Here are some tips for finding support:
- Look for Rainbow Tick-accredited clinics in your area.
- Ask potential providers if they are LGBTIQ+ inclusive and trauma-informed.
- Reach out to community groups or forums for recommendations — peer support can be gold.
- If you’re seeing a psychologist, they can write a support letter to help advocate for your needs during medical appointments or procedures.
Final thought: There’s no wrong way to do menopause.
Whether you’re powering through with barely a symptom, or you’ve got a fan in one hand and a heat pack in the other, you’re not broken.
You’re not alone.
And the more we talk about menopause – loudly, openly, and from our own queer perspectives – the less isolating it becomes.
Let’s keep the conversation going.
Some handy links:
Menopause doesn’t mean the end of sex — but it might mean a different relationship to pleasure, sensation, and desire.
Where to
find support
Looking for someone to talk to?
Access safe (and pre-screened) health from our resource list.