Blood, Sweat and Queers: Understanding Menstrual Health

Periods. For some of us, they can feel affirming, a sign that our bodies are doing their thing. For others, they can bring pain, discomfort, dysphoria or just the hassle and frustration of dealing with them every month.
However you experience them, learning more about your cycle can make it a little easier to navigate.
If you’ve got questions like….
- What’s happening with my hormones during my cycle?
- How can I manage menstrual pain?
- How do I track my cycle — and why would I want to?
- Where can I access free pads or tampons?
- How does gender-affirming hormone therapy affect periods?
- Are my premenstrual symptoms normal?
- What’s the difference between PMS and premenstrual dysphoric disorder (PMDD)?
- Sapphic relationships: am I cycle syncing with my partner?
… you’re in the right place. Read on for our queer-friendly guide to menstrual health.
Respectfully…what is happening during my menstrual cycle?
Here’s a short video from Sexual Health Victoria for a quick refresher of the basics.
The menstrual cycle is much more than just bleeding. It’s a collaboration between your brain, ovaries, and uterus. Hormones rise and fall throughout the month, influencing everything from energy and mood to focus and sex drive.
Menstruation & the Follicular Phase
(Approx. Days 1–13, but it varies)
Day 1 of your cycle kicks off when bleeding begins — the uterus lining is shedding, and your period is in full swing. This usually lasts between 3–7 days and can come with cramps, fatigue, and low energy.
But there’s good news: as oestrogen levels begin to rise, many people start to feel relief from premenstrual symptoms and a gradual boost in mood and energy. Around this time, your brain signals the ovaries to prepare for ovulation — setting the stage for the next phase.
Side note: Some forms of hormonal contraception can safely reduce, delay or completely stop periods. Head to Birth Control Beyond the Binary for more info.
Ovulation
(Around Day 14, give or take)
Hormones like LH (luteinising hormone) and FSH (follicle-stimulating hormone) surge to trigger the release of an egg from the ovaries. For many, this is when energy peaks, mental clarity sharpens, and sex drive gets a boost. This can also come with some cramps and bloating.
The “fertile window”
If avoiding or getting pregnant is relevant for you, it helps to know about the fertile window. It’s the time in your cycle when pregnancy is most likely if sperm is present.
- It usually lasts about 6 days.
- It begins up to 5 days before ovulation (since sperm can survive in the reproductive tract for several days).
- It includes the day of ovulation itself, when the ovary releases an egg.
- Once released, an egg can only be fertilised for about 12–24 hours.
After this window closes, pregnancy is less likely until the next cycle begins.
Luteal Phase
(Post-ovulation to the start of your next period)
Here’s where PMS (premenstrual syndrome) tends to show up, thanks to rising progesterone and fluctuating oestrogen. You might feel mood swings, bloating, breast/chest tenderness, irritability, or just plain exhausted.
Some folks feel more inward or reflective during this time, others feel like setting their phone on fire. If you’re finding this part of your cycle particularly difficult, it’s important to take your symptoms seriously and speak to your GP.
How can I manage menstrual pain?
While your period is in full swing, the uterus contracts to help shed its lining. These contractions are triggered by prostaglandins, hormone-like substances that also cause inflammation and pain.
Mild to moderate cramps during your period are common, especially in the first couple of days of bleeding. You might feel pain in your lower abdomen, lower back, hips and inner thighs
While this can definitely be uncomfortable, for most people it’s manageable enough with some rest and some of the options below.
- Exercise and gentle movement: Regular exercise can reduce cramps and improve mood. During your period, light stretching, yoga, or a short walk might ease pain — but rest when you need to.
- Over-the-counter pain relief: Over-the-counter options include ibuprofen, naproxen, paracetamol, and Buscopan. NSAIDs (Non-Steroidal Anti-Inflammatory Drugs ibuprofen, naproxen) can work more effectively if started 1–2 days before your period and continued for the first few days. Always follow dosage instructions, take the tablets with food and check with a pharmacist or GP if unsure.
- Heat: Using a heat pack or taking a warm bath can help relax your muscles and lessen the impact of cramps.
- TENS machine: A small device that sends mild electrical pulses to block pain and release endorphins. Drug-free, safe for most people, and most effective at the first sign of cramps. You can buy these from a chemist or online.
- Period tracking: Knowing when your period is due helps you prepare — whether that’s keeping pain relief handy, adjusting plans, or giving yourself more rest.
Severe period pain is not something you should just put up with. If the pain makes it hard to do your daily activities, sleep or move around, it’s a good idea to see your doctor.
What is Period Tracking?
If you find yourself coming up blank when your doctor asks when your last cycle was, you might want to try period tracking.
Put simply, it means logging your symptoms each cycle. You can use an app, a notebook or just your notes app.
Why should I track my periods?
- Pain prevention: Some pain relief strategies (like NSAIDs or TENS machines) work best if started before cramps begin. Tracking helps you stay one step ahead.
- Mood management: Need to have a tough convo with a significant other? Maybe pencil that in for later in your cycle. Understanding your cycle can help you plan for times when you might need extra care and rest.
- Fertility awareness: If you’re trying to conceive, avoid pregnancy, or just learn more about your body, tracking can help you understand your body better.
- Overall health: Everyone’s cycle is a little different, and period tracking can help you work out what’s normal for you. It can also be a marker of your overall health. Irregular periods, missed cycles, or sudden changes might be worth checking with a doctor.
How to period track
- When your period starts and ends
- How long your cycle is (from day 1 of bleeding to the day before your next period)
- Write down symptoms like flow heaviness, nausea, pain, and mood changes that you notice over the course of your cycle.
Your period might change as you move through life (i.e. during perimenopause), but if you notice anything concerning, read on for extra support.
When to get help with period symptoms
Because menstruation has been treated with shame and silence for so long, many of us don’t take our pain seriously or feel dismissed when we do.
If you’re unsure whether to get more support, here are some signs that you should:
Red flags:
- Bleeding heavily — soaking through a pad or tampon every 1–2 hours, passing large clots (bigger than a 50-cent coin), or bleeding for more than 7 days
- Severe pain that affects your work, sleep, or daily activities — and doesn’t ease with over-the-counter meds
- Skipping periods for several months (unless it’s expected, e.g. due to hormonal contraception)
- Periods that are too frequent (e.g. every 2 weeks) or too far apart (e.g. more than 35–40 days)
- Significant mood swings, depression, dysphoria, or anxiety linked to your cycle
If your current doctor doesn’t feel like a supportive option, check out clinics that understand queer and trans health. Sexual Health Victoria is Rainbow Tick approved and offers Telehealth .
What’s the difference between pre-menstrual symptoms (PMS) and premenstrual dysphoric disorder (PMDD)?
About 80% of people who menstruate will get PMS in the days or weeks before their period. It’s a normal and common experience, linked to the hormonal changes that happen in the luteal phase.
There might be signs like:
Physical symptoms: bloating, headaches, breast tenderness, cramps, fatigue.
Emotional / mental symptoms: mood swings, irritability, anxiety, low mood, difficulty concentrating.
Behavioural symptoms: changes in sleep, appetite, or energy levels.
While these can be uncomfortable and frustrating, they shouldn’t majorly disrupt your day-to-day life. Especially after some extra rest and the pain management tips above.
On the other hand, about 3-8% of people who menstruate experience PMDD. While some of the symptoms share some overlap with PMS, PMDD symptoms are much more intense. This includes severe depression, anxiety, anger, mood swings, brain fog and sometimes suicidal thoughts. It’s a recognised psychiatric disorder that severely impacts relationships, work, study and daily life.
As with PMS, these symptoms will show up during the luteal phase and then usually disappear once bleeding starts.
If you’re looking for more info to understand the difference between PMS and PMDD:
- Here’s a PMDD factsheet from Jean Hailes tailored for cisgender lesbian, bisexual and queer women.
- We had a chat with queer sexologist, Kendall Buckley, to learn more about how PMDD can affect LGBTIQ+ women and gender diverse people.
- This video from LGBTIQ+ Health Australia explores lived experience and clinical perspectives on how these conditions are experienced, understood and managed by our communities
As always, it’s really important to speak to your doctor if your pre-menstrual phase is causing you major problems each month.
If you suspect PMDD, it can help to read up on the condition and track your cycles to help your doctor with the diagnosis process.
How can gender-affirming hormone therapy (GAHT) affect menstruation?
If you’re taking oestrogen-based GAHT and you were presumed male at birth:
Oestrogen can cause your body’s hormonal rhythms to shift in ways that affect mood and energy. You might notice some PMS-like symptoms like nausea, bloating, food cravings and mood swings.
Some find period tracking, prioritising rest, and extra self-care helpful during these times.
If you’re taking testosterone GAHT and you were presumed female at birth:
Testosterone often causes periods to become lighter, less frequent, or stop altogether.
Important note: Even if your bleeding stops, pregnancy is still possible if you have a uterus and are having sex with someone who produces sperm. Contraception is still important if pregnancy isn’t part of your plan.
For more on the relationship between testosterone GAHT and menstrual changes, check out Trans Health Research for evidence-based information.
Tampon Tax: What If I Can’t Afford Period Products?
Three in five people with periods have struggled to afford period products. If this is you, you’re not alone.
Good news for Victorians:
In 2025, over 1,450 machines dispensing free period products will be installed at up to 700 sites.
Find a pad and tampon dispensing machine with this handy map visualiser.
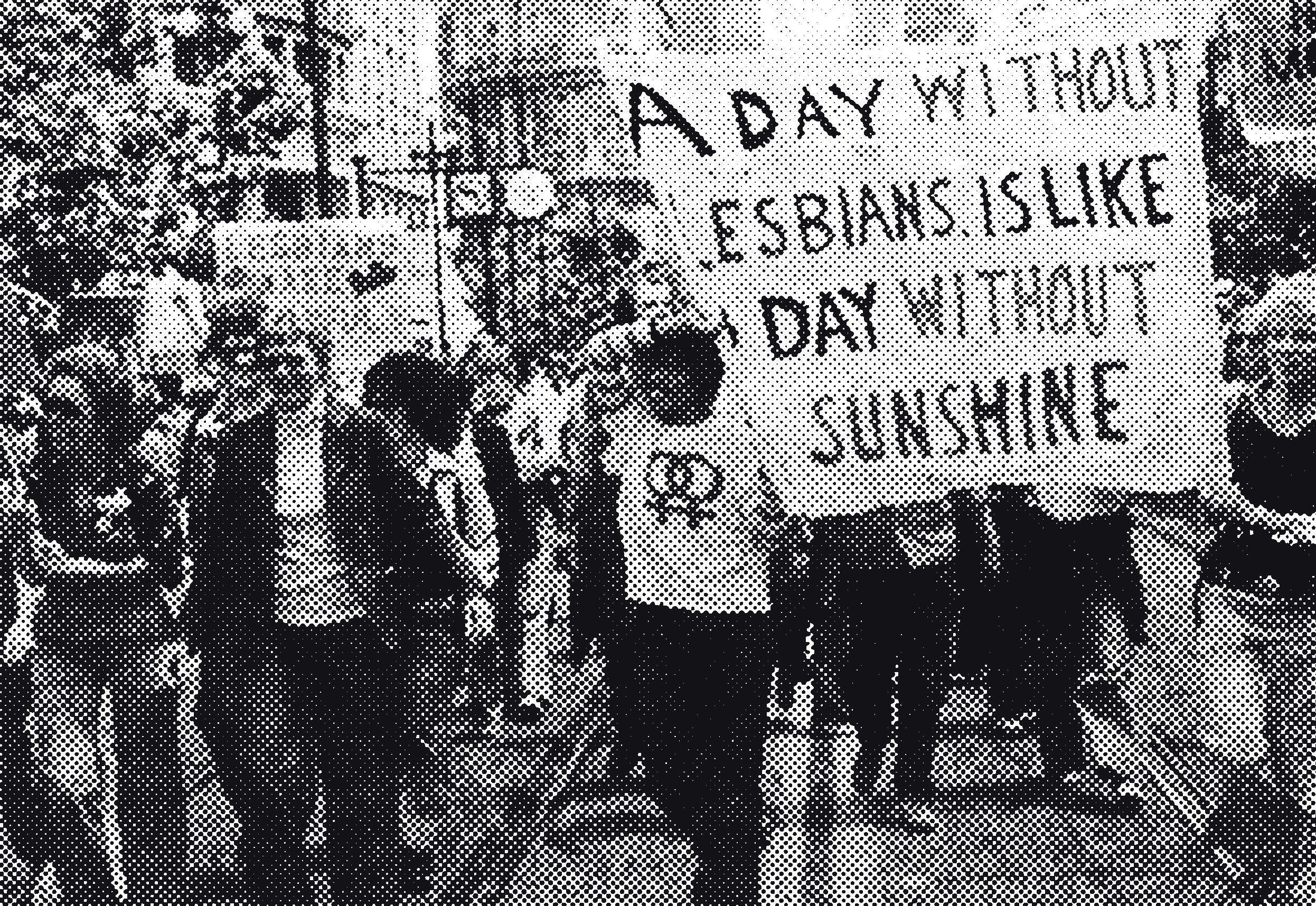
Am I Cycle-Syncing With My Partner?
For those of us in relationships where more than one person has a uterus, periods can come with unique pros and cons. Sure, it can be rough if PMS hits you both at the same time, but sharing painkillers, period products, heat packs, and chocolate is a certain kind of sapphic medicine.
But what about the idea of cycle syncing — when partners’ periods supposedly line up. Many of us swear it happens, but what does the science say?
While some of us can attest to syncing with our significant other(s), a new joint study by period tracking app Clue and Oxford University claims to have debunked this phenomenon.
Clue surveyed users about their experiences of synced periods — asking about their relationships, whether they lived together, and whether anyone was using hormonal contraception. From over 1,500 responses, researchers identified 360 pairs of users who had logged at least three cycles in the same timeframe.
Here’s what they found:
- 273 pairs had cycles that drifted further apart over time
- Only 79 pairs had cycles that actually moved closer together
So while the idea of syncing might feel true to our experience, the data doesn’t back it up — at least not in this study.
Still, if you’re a cycle syncing believer, don’t worry — this is just one study, and research in this area is very limited.
Maybe some sapphic mysteries aren’t meant to be solved?
Where to
find support
Looking for someone to talk to?
Find peer groups, community organisations and referral pathways for LGBTIQ+ women and gender diverse people.